
As healthcare costs have come under increased scrutiny over the past several years, policymakers have increasingly realized that the reduction of the amount and kind of services used is an even more important cost-control measure than the simple reduction of prices. This reduction in the amount and kind of services ultimately implies that policymakers would like physicians (such as anesthesiologists, cardiologists, etc.) to reduce their utilization of healthcare resources by reducing the number of diagnostic tests they order, which drugs they prescribe, which surgical and other procedures they perform, and at what facilities they perform these procedures. However, since physicians ultimately dictate the utilization of healthcare resources implementation of these cost-control measures is quite difficult, and instead of direct control over physicians, policymakers must exert cost-control measures by altering incentives. To this end, the Affordable Care Act implemented many new policies aimed at changing payment incentives. Chief amongst these policies is changing payment away from a fee-for-service model through the creation of accountable care organizations (ACOs).
Simply put, ACOs are networks of physicians or physicians, hospitals, and other providers that take both clinical and financial responsibility for the care of patients. ACOs aim to breakdown barriers between primary care physicians, specialists, hospitals, home health care agencies, hospices, pharmacies, and other providers; the idea behind this organization is to coordinate patient care-particularly for patients suffering from chronic illnesses (who account for the majority of costs)-to focus on high-quality, lower-cost interventions and not just on what services are paid for. This organization would reduce wasteful duplication of tests and unnecessary interventions, while keeping patients healthy and reducing the need for treatments, specialist referrals, emergency room visits, and long-term hospitalizations.
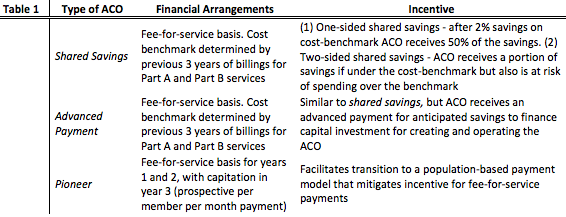
While there are many conditions for a healthcare organization, such as an anesthesia management company, to qualify as an ACO (e.g. care for 5,000 Medicare beneficiaries, 3 year agreement with Medicare, CMS quality reporting, physician-led governance, etc.), ACOs aim to reduce healthcare costs by altering how payments for services are distributed. With the passing of the Affordable Care Act, the Medicare program was authorized to adopt the ACO model and with it three different types of ACO models were created. These types are summarized in Table 1.
While the most common ACO model is the shared savings, many worry that the initial reliance on fee-for-service payments may still encourage physicians to order more tests, visits, and treatments in order to increase payment. Furthermore, since ACOs entail significant start-up costs for integrated electronic health records, disease registries, effective care management programs, telemedicine, and other monitoring mechanisms. Since the deployment of these technologies and programs incur high costs, effective management others continue to worry that ACOs will ultimately fail due to lack of the appropriate financial and human resource management. The last major concern with ACOs are that through creation of large, comprehensive care delivery groups, Medicare may decrease competition among physicians and hospitals; ACOs, rather, than engage with Medicare, may negotiate better rates with private insurers and thus eliminate any savings for the overall healthcare system. Regardless of the concerns over ACOs, the ACO model has undoubtedly taken off-the first quarter of 2016 recorded a record 838 ACO organizations distributed across the three models and spurred use of the ACO model amongst private insurers.

