
Meaningful use is defined as using certified electronic health record (EHR) technology to “improve quality, safety, efficiency, and reduce health disparities,” as well as to help engage patients and their families, improve care coordination and public health, and ensure security and privacy of private patient health information [1]. It is hoped that if all eligible professionals comply with meaningful use, then there will be better clinical and population health outcomes, as well as increased transparency and efficiency, more empowered individuals, and more robust health systems research [1]. There are three stages of meaningful use. The first stage was rolled out from 2011-2012 and involved data capture and sharing. The second stage was implemented in 2014 and involved advancing clinical processes [2]. The second stage introduced new objectives and higher thresholds, “requiring providers to extend EHR capabilities to a larger portion of their patient populations” [2]. The third stage was scheduled to begin in 2014 but has been pushed back to begin in 2017 instead. The goal of this third stage is to “simplify the program, drive interoperability between electronic health records, and improve patient outcomes” [2].
Where did this idea of meaningful use come from? The American Reinvestment & Recovery Act (ARRA) of 2009 included many provisions to modify health infrastructure, including the Health Information Technology for Economic and Clinical Health (HITECH) Act, which supports the concept of EHR meaningful use [3]. The Centers for Medicare & Medicaid Services (CMS) and the Office of the National Coordinator for Health IT (ONC) have led the push for implementation of EHR meaningful use [3]. CMS even provides incentive payments to eligible hospitals (EHs) and eligible professionals (EPs) who can show that they have attempted to adopt, implement, or upgrade certified EHR technology [3]. With the rollout of stage 3, EPs and EHs who fail to meet certain requirements will have their Medicare payments adjusted downward [3]. These measures have been met with some backlash, as such penalties are seen as controversial. Thus there has been much conversation about stage 3 and the future of meaningful use. In particular, anesthesiologists and anesthesia management companies have taken issue with meaningful use, noting that they would have to “fit a square peg in a round hole” in order to meet the meaningful use requirements [6].
However, meaningful use requirements do not apply to anesthesiologists in the same way that they do to other physicians. Any physician who has the designation of “anesthesiology” in the Medicare Provider Enrollment Chain and Ownership System is exempt from the meaningful use requirements [4]. However, anesthesiologists who satisfy the requirements of meaningful use can still qualify to receive the incentive payments from CMS [4]. These stipulations apply only to physicians who practice anesthesiology; CRNAs are not classified as “eligible professionals” under the meaningful use program [4]. Anesthesia information management systems (AIMS) have been used by anesthesia service providers to document the physiology and interventions of their patients for over thirty years [5]. While the Anesthesia Patient Safety Foundation recommends the use of AIMS to improve patient safety, a 2011 survey found that only 24% of US anesthesiologists were using AIMS with an addition 13% planning to install it in the near future [5]. While EHR, including AIMS, adoption rates have increased since 2011, it is key that implementation rates continue to increase as widespread EHR use can improve care quality through “automated documentation of physiologic monitoring [and] optimizing quality and performance with clinical decision support applications for the patient and OR as a whole” [5]. However, the ultimate goal of widespread EHR use is that the data can be used to track population health to eventually guide quality improvement initiatives [5].
What does the future look like for meaningful use? In January 2016, CMS Acting Administrator Slavitt said that meaningful use was “effectively over” and would be “replaced with something better,” namely the EHR component of the Merit-Based Incentive Payment System (MIPS) which would “measure and compensate physicians on four distinct elements: quality, practice improvement, cost, and use of technology” [4]. While many aspects of meaningful use will be included within MIPS, the new program will pay physicians to use technology to improve outcomes rather than rewarding doctors for just using the technology [4]. However, this new program is not planned to go into effect until at least 2019. Regardless of the form in which meaningful use is implemented, it is important to recognize that meaningful use is not a static target and rather we must continue to amend our systems and goals in order to ensure that our patient information is as secure as possible and that we can use the data that an EHR can provide to improve population health in the best way possible.
[1] https://www.healthit.gov/providers-professionals/meaningful-use-definition-objectives [2] http://www.athenahealth.com/knowledge-hub/meaningful-use/stages [3] http://www.cdc.gov/ehrmeaningfuluse/introduction.html [4] http://www.anesthesiallc.com/publications/anesthesia-industry-ealerts/866-meaningful-use-update-for-anesthesiologists-and-pain-physicians-hardship-exception-application [5] Galvez, J.A., et al (2015). A Narrative Review of Meaningful Use and AnesthesiaInformation Management Systems. Anesthesia & Analgesia, 121(3), 693-706.
[6] https://ahsrcm.com/assets/Anesthesia-and-Meaningful-Use.pd

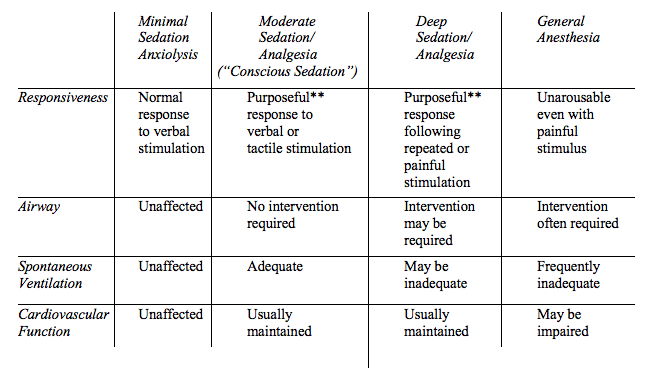 Controversy exists regarding whether non-anesthesia providers are capable of ensuring patient safety in the face of the above concerns. While some retrospective studies have demonstrated a low incidence of cardiopulmonary complications with gastroenterologist-directed administration of drugs with narrow safety margins such as propofol, confounding factors and a lack of prospective randomized trials make current evidence insufficient. What can be said is that patients are often more obese with more complex comorbidities than those endoscopists encountered decades ago, and a dedicated anesthesia provider is uniquely qualified for recognizing and intervening upon common complications of sedation for endoscopy: airway obstruction, apnea, aspiration and hypotension.
Controversy exists regarding whether non-anesthesia providers are capable of ensuring patient safety in the face of the above concerns. While some retrospective studies have demonstrated a low incidence of cardiopulmonary complications with gastroenterologist-directed administration of drugs with narrow safety margins such as propofol, confounding factors and a lack of prospective randomized trials make current evidence insufficient. What can be said is that patients are often more obese with more complex comorbidities than those endoscopists encountered decades ago, and a dedicated anesthesia provider is uniquely qualified for recognizing and intervening upon common complications of sedation for endoscopy: airway obstruction, apnea, aspiration and hypotension.

