
Upper and lower endoscopies are among the most prevalent procedures performed in the US today. While historically sedation has been provided by endoscopists with the assistance of nursing staff, over the past decade there has been an increase in the involvement of anesthesia services, particularly for patients with complex comorbidities or need for deeper sedation. As sedation and anesthesia for GI endoscopy evolves, there is ongoing debate and emerging research on the safety and outcomes of various drug regimens and their administrators.
Not all endoscopy procedures are equivalent. The sedation required for routine colonoscopy or sigmoidoscopy is generally less than that required for an upper endoscopy, and more advanced procedures such as endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasonography (EUS) and balloon endoscopy require an even deeper plane of anesthesia. Factors in choosing the level of anesthesia include procedural needs (e.g. immobility for EUS with fine needle biopsy), patient comorbidities and patient’s degree of cooperativeness/pain tolerance.
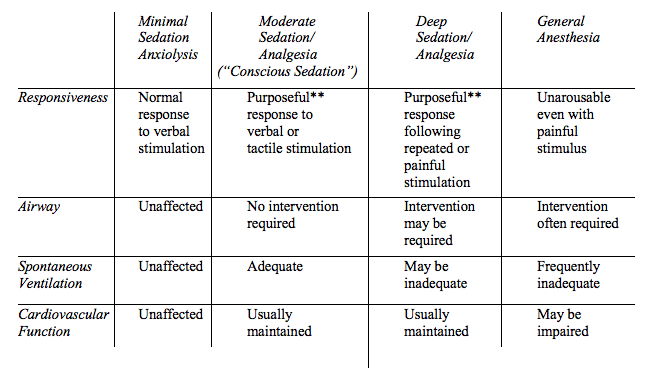
Below is a description of the sedation continuum as defined by the American Society of Anesthesiologists. A provider targeting one level of sedation should be prepared to manage the next level deeper. Therefore while most routine GI endoscopies can be performed under moderate or “conscious” sedation, it is important for the responsible provider to be able to react to airway compromise, interruptions in spontaneous ventilation, and cardiovascular instability.
 Controversy exists regarding whether non-anesthesia providers are capable of ensuring patient safety in the face of the above concerns. While some retrospective studies have demonstrated a low incidence of cardiopulmonary complications with gastroenterologist-directed administration of drugs with narrow safety margins such as propofol, confounding factors and a lack of prospective randomized trials make current evidence insufficient. What can be said is that patients are often more obese with more complex comorbidities than those endoscopists encountered decades ago, and a dedicated anesthesia provider is uniquely qualified for recognizing and intervening upon common complications of sedation for endoscopy: airway obstruction, apnea, aspiration and hypotension.
Controversy exists regarding whether non-anesthesia providers are capable of ensuring patient safety in the face of the above concerns. While some retrospective studies have demonstrated a low incidence of cardiopulmonary complications with gastroenterologist-directed administration of drugs with narrow safety margins such as propofol, confounding factors and a lack of prospective randomized trials make current evidence insufficient. What can be said is that patients are often more obese with more complex comorbidities than those endoscopists encountered decades ago, and a dedicated anesthesia provider is uniquely qualified for recognizing and intervening upon common complications of sedation for endoscopy: airway obstruction, apnea, aspiration and hypotension.
Drug regimens used for sedation during GI endoscopy generally fall under two categories: a combination of benzodiazepine and narcotic (e.g. midazolam and fentanyl) and propofol as a bolus and/or infusion. In the United States, the former has been traditionally administered by gastroenterologists, the latter by anesthesiologists. Propofol has the advantage of achieving deep sedation with reliable and rapid onset, and has been borne out in research studies to have superior recovery times and overall patient and physician satisfaction. However, it is less forgiving than benzodiazepine/narcotic regimens given its narrow therapeutic window before encountering hypotension and apnea. Furthermore it lacks a reversal agent such as flumazenil or naloxone which can rapidly rescue overdose of these other agents.
The American Society for Gastrointestinal Endoscopy recommends providers administering propofol sedation possess specific training on the properties and use of this drug, as well as expertise in emergency airway management. Personnel should be dedicated to monitoring the patient’s airway and ventilation, with capnography strongly encouraged.
While ASGE guidelines do not require an anesthesiologist perform these functions during propofol sedation, it is a point of contention whether adequate monitoring and airway management can be provided by the gastroenterologist performing the procedure or nursing staff who may be juggling multiple tasks. The attention and experience required to detect airway and hemodynamic instabilities, which can present with an insidious onset prior to decompensation, and the skill set necessary to quickly perform high quality mask ventilation, insert advanced airway devices, manage blood pressure abnormalities and tailor sedation regimens to complex patient comorbidities is uniquely suited to the skill set of a dedicated anesthesiologist. Reliance on alarms is far from foolproof, for capnography is less reliable in upper endoscopies given carbon dioxide escape from a necessarily open system as the mouth is accessed, and pulse oximetry has a dangerous lag time between apnea and registered desaturation.
Despite these concerns, the existing evidence – albeit imperfect – has not lent much weight to fears for patient safety during non-anesthesia administration of propofol sedation. Biases in study conduction, publication, patient population and sampling are among the variables that must be examined when these data are scrutinized. What can be said for certain is that the role of anesthesia services in GI endoscopy will continue to be a topic of debate and evolution, and it behooves all parties to be well apprised of current practice and incoming research.
References:
- Goudra B, Singh PM. Anesthesia for gastrointestinal endoscopy: A subspecialty in evolution?Saudi Journal of Anaesthesia. 2015;9(3):237-238. doi:10.4103/1658-354X.154691.
- http://www.asge.org/uploadedFiles/Publications_and_Products/Practice_Guidelines/Sedation%20and%20Anesthesia%20in%20GI%20Endoscopy%202008.pdf
- Vaibhav Wadhwa, Danny Issa, Sushil Garg, Rocio Lopez, Madhusudhan R. Sanaka, John J. Vargo. Similar Risk of Cardiopulmonary Adverse Events Between Propofol and Traditional Anesthesia for Gastrointestinal Endoscopy: A Systematic Review and Meta-analysis. Clinical Gastroenterology and Hepatology. Available online 21 July 2016, ISSN 1542-3565, http://dx.doi.org/10.1016/j.cgh.2016.07.013.

