The management of the difficult airway is a topic both ubiquitous and enigmatic in the realm of clinical anesthesia care. Like the famous Justice Stewart quote, you know it when you see it, but no one has a hard and fast definition of what it is. Commonly it’s characterized as a clinical situation in which a conventionally trained anesthesiologist has difficulty with mask ventilation, intubation, or both. How each practitioner chooses to approach such situations, both expected and unexpected, varies based on whom you ask. Even among the world’s airway experts there are patterns of agreement, but no clear rules on how to handle airway management.
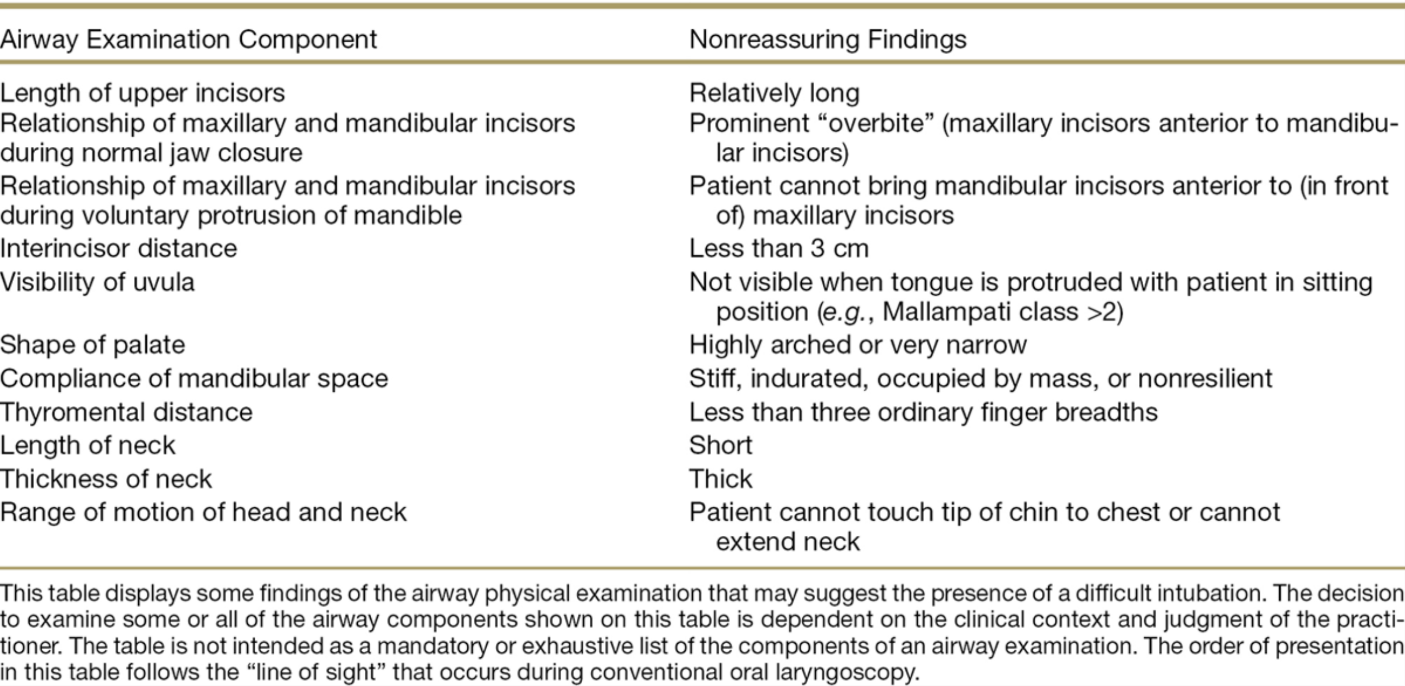
The first step of difficult airway management is recognition and preparation. Red flags in the patient’s history (previous difficult mask/intubation, obstructive sleep apnea, head and neck radiation, mediastinal mass, ankylosing spondylitis to name a few) and physical exam (table below) should be reviewed whenever possible and adequate preparation made for cannot ventilate/cannot intubate scenarios.
Informing the patient of possible difficulties involving airway management, having an extra pair of hands if possible, ensuring adequate preoxygenation, and actively pursuing avenues to continue delivering supplemental oxygen for the duration of airway management (via nasal cannula, LMA, insufflation, etc) are part of the basic preparation recommended by the ASA. Choosing appropriate avenues to secure the airway is based upon provider familiarity and specific patient circumstance, and includes but is not limited to video laryngoscopy, fiberoptic intubation, and light wand. Perhaps more important than how to intubate the patient is to decide whether to perform intubation after induction or awake. Choosing the former without convincing evidence of the ability to mask ventilate would be difficult to defend should adverse consequences occur.
In spite of adequate preoperative assessment, unanticipated difficult airways are still encountered and can have devastating consequences. Reference to the difficult airway algorithm below is helpful in systematically attempting to establish adequate ventilation and/or intubation.
References:
Apfelbaum, JL et al. Practice Guidelines for Management of the Difficult Airway: An Updated Report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 02 2013, Vol.118, 251-270.