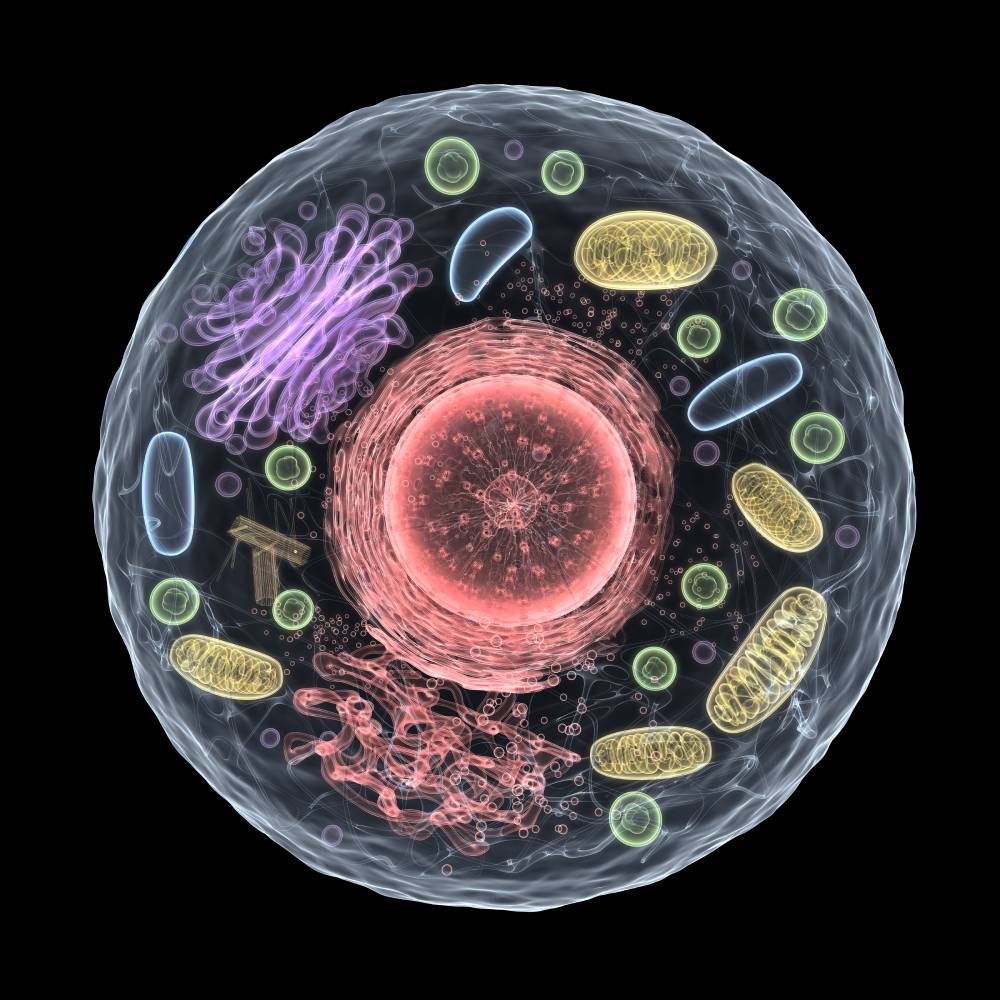
Oxygen is essential for the survival and proper functioning of most eukaryotic organisms, including humans [3]. It plays a vital role in cellular respiration, the process by which cells generate energy by breaking down glucose and other nutrients. Cells have highly evolved systems for sensing and responding to having too little oxygen [3]. At the cell membrane, specialized ion channels on the cell membrane, particularly K+ channels, are responsible for the detection of oxygen, while several oxygen-responsive transcription factors inside the cell drive the molecular responses to hypoxia [9]. Lack of oxygen or excessive oxygen consumption could result in inadequate oxygen supply at the tissue or cellular level to sustain appropriate homeostasis, a condition defined as hypoxia [2,3]. Several factors can contribute to hypoxia, including various conditions, such as respiratory disorders, cardiovascular diseases, anemia, and high altitudes [6,9]. If hypoxic conditions are sustained, it can lead to a metabolic crisis that is ultimately lethal to cells and results in several detrimental outcomes if left untreated.
Reduced energy generation is one of the most direct repercussions of cells receiving too little oxygen. Cellular respiration needs oxygen to make ATP, the cell’s energy currency.4 However, during hypoxic conditions, ATP-consuming processes are inhibited, and metabolism is disrupted until oxygen homeostasis is restored [4]. When cells cannot create energy through cellular respiration, they may turn to alternate metabolic pathways that are often less effective and generate toxic byproducts [13]. These byproducts can accumulate in the cell and cause damage, leading to cell death [13].
Too little oxygen in cells can also cause inflammation and oxidative stress [8]. Oxygen acts as the last electron acceptor in oxidative phosphorylation [8]. Reactive oxygen species (ROS) are normal byproduct of oxidative phosphorylation, but during cellular hypoxia, ROS production may become unbalanced, leading to an overabundance of these molecules [8]. ROS accumulation may increase the susceptibility of cells to degeneration, resulting in inflammation, oxidative stress, and other forms of cellular damage [8]. This damage can inhibit the cell’s ability to self-repair, which may result in cell dysfunction or death [8].
Oxygen is also essential for the proper functioning of the immune system, including neutrophils and monocytes [7,12]. Without enough oxygen, the immune system may not function optimally, resulting in a compromised immune system and potentially leading to an increased susceptibility to infection and other disorders [5]. Hypoxia can also affect the production of cytokines, which are proteins that help to regulate the immune response [9]. When the body is hypoxic, the production of specific cytokines may be reduced, leading to an impaired immune response [9].
The effects of too little oxygen on cells and the body can vary depending on the severity and duration of the condition. In mild instances, symptoms include shortness of breath, tiredness, and headache [2]. However, severe or prolonged hypoxia requires immediate medical attention and may result in organ damage and failure, coma, and even death [2]. It is important to address and treat hypoxia as quickly as possible to minimize the potential for cellular damage and the associated negative consequences. Treatment may involve oxygen therapy, medications, or addressing any underlying conditions contributing to the hypoxia. Early diagnosis and treatment can help to prevent further complications and improve the chances of a full recovery.
References
- Abe, H., Semba, H., & Takeda, N. (2017). The Roles of Hypoxia Signaling in the Pathogenesis of Cardiovascular Diseases. Journal of atherosclerosis and thrombosis, 24(9), 884–894. https://doi.org/10.5551/jat.RV17009
- Bhutta BS, Alghoula F, Berim I. Hypoxia. [Updated 2022 Aug 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482316/
- Chen, P. S., Chiu, W. T., Hsu, P. L., Lin, S. C., Peng, I. C., Wang, C. Y., & Tsai, S. J. (2020). Pathophysiological implications of hypoxia in human diseases. Journal of biomedical science, 27(1), 63. https://doi.org/10.1186/s12929-020-00658-7
- Lee, P., Chandel, N. S., & Simon, M. C. (2020). Cellular adaptation to hypoxia through hypoxia inducible factors and beyond. Nature reviews. Molecular cell biology, 21(5), 268–283. https://doi.org/10.1038/s41580-020-0227-y
- Maggini, S., Pierre, A., & Calder, P. C. (2018). Immune Function and Micronutrient Requirements Change over the Life Course. Nutrients, 10(10), 1531. https://doi.org/10.3390/nu10101531
- Mozos I. (2015). Mechanisms linking red blood cell disorders and cardiovascular diseases. BioMed research international, 2015, 682054. https://doi.org/10.1155/2015/682054
- Palazon, A., Goldrath, A. W., Nizet, V., & Johnson, R. S. (2014). HIF transcription factors, inflammation, and immunity. Immunity, 41(4), 518–528. https://doi.org/10.1016/j.immuni.2014.09.008
- Semenza G. L. (2012). Hypoxia-inducible factors in physiology and medicine. Cell, 148(3), 399–408. https://doi.org/10.1016/j.cell.2012.01.021
- Taylor A. T. (2011). High-altitude illnesses: physiology, risk factors, prevention, and treatment. Rambam Maimonides medical journal, 2(1), e0022. https://doi.org/10.5041/RMMJ.10022
- Taylor, C. T., & Colgan, S. P. (2017). Regulation of immunity and inflammation by hypoxia in immunological niches. Nature reviews. Immunology, 17(12), 774–785. https://doi.org/10.1038/nri.2017.103
- Trayhurn P. (2019). Oxygen-A Critical, but Overlooked, Nutrient. Frontiers in nutrition, 6, 10. https://doi.org/10.3389/fnut.2019.00010
- Zenewicz L. A. (2017). Oxygen Levels and Immunological Studies. Frontiers in immunology, 8, 324. https://doi.org/10.3389/fimmu.2017.00324
- Zorov, D. B., Juhaszova, M., & Sollott, S. J. (2014). Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiological reviews, 94(3), 909–950. https://doi.org/10.1152/physrev.00026.2013

