Twenty-one millionpeople in the U.S.will receivegeneralanesthesiain a typical year.But the ability toartificially induce any of the defining components—analgesia (insensitivity to or prevention of pain), paralysis, amnesia, and sedation/unconsciousness—is relatively new. The word anesthesia itself only first appeared in the dictionary in 1751, and was first used to describe the mental state that follows from the inhalation of ether vapor by the prominent physician, Oliver Wendell Holmes, Sr.
Only 300 years ago, surgical pain relief options were limited to the consumption of alcohol or opium (to the point of stupor), or the powers of suggestion or “positive thinking”. Magnets and hypnosis, or ‘Mesmerism’ were used to cure various ailments. Around May 1812,the English novelist Fanny Burney wrote a compelling account of her experience undergoing a mastectomy without anesthesia:
“I saw the glitter of polished Steel – I closed my Eyes. I would not trust to convulsive fear the sight of the terrible incision. Yet – when the dreadful steel was plunged into the breast…I needed no injunctions not to restrain my cries. I began a scream that lasted unintermittingly during the whole time of the incision – & I almost marvel that it rings not in my Ears still [?] so excruciating was the agony. When the wound was made, & the instrument was withdrawn, the pain seemed undiminished..I concluded the operation was over – Oh no! presently the terrible cutting was renewed – & worse than ever”
In contrast, the gratitude felt by the first mother to receive chloroform for the delivery is clearly expressed by the name she gave her baby—Anaesthesia.
Anesthesia Through the Ages
At Xenon Health, anesthesia is our specialty.But how did our field progress from the prescribing of a few shots of whiskey prior to surgery to the precise science of administering by gas, injection, and infusion drugs that act on different and overlapping sites in the central nervous system? This post reviews the landmark discoveries that led to the evolution of anesthesia over the centuries, and pays homage to the innovators that shaped the field.
400 BC
- Hippocrates recommends opium poppy use for pain-relief.
13thCentury
- Theodoric of Lucca, an Italian physician and bishop, induces unconsciousness prior to surgery by holding sponges soaked with opium, mandrake, and hemlock under patients’ noses.
- In 1275, the Spanish chemist Raymundus Lullius synthesizes ether, which would become the first reliable, general anesthetic—though this would not be recognized for almost570 years.
16th Century
- Ether is first used on animals by Paracelsus in 1525. Fifteen years later, Valerius Cordus repeats Lullius’ synthesis by distilling ethanol and sulfuric acid.
- In Malta, patients to be operated on were made unconscious with a wooden hammer.
17th Century
- Opium is first administered intravenously.
18th Century
- In 1745, the French explorer Charles-Marie de La Condamine publishes the first written account ofcurare, a paralytic poison derived from a plant that he observes is used on arrows by South American tribes to kill their prey. Note: This property will become important in 200 years as future anesthesia techniques will require the control of muscle relaxation.
- Nitrous oxide (NO), commonly known as laughing gas, is isolated by Joseph Priestley in 1772.This substance became a heavily researched topic, with Dutch chemist Martinus van Marum publishing 35 papers on his studies and the nitrous oxide experiments performed during the last years of the century by Thomas Beddoesand Humphry Davy demonstrating the gas could be inhaled with analgesic effects.
- The engineer James Watt makes two related inventions—a machine to produce NO and a “breathing apparatus” to inhale the gas.
- In 1778, Antoine Lavoisierdiscovers oxygen (O2).
19th Century
- In 1805, morphine is discovered by Friedrich Serturner, who names it after the Greek god of dreams, Morpheus. It becomes the first product launched by Merck in 1827.
- Chloroform is simultaneously discovered in 1831 by scientists in three countries. Although frequently used for about 50 years after it is discovered to have anesthetic properties in 1847, a concern about fatalities emerged just 2 months after it is introduced. It was later found to cause death from paralysis of the heart in about 1/3000 patients (and also to be toxic to the liver and to depress most other organs) and by 1940, was replaced by safer alternatives.
- General anesthesia is officially born in1842, with William E. Clarke administering ether from a towel to a patient about to undergo a tooth removal. Its first documented use as a gas for surgical pain relief is by Crawford W. Long, but since he waited to publish this until 1849, the credit was instead attributed to a Boston dentist, William Morton. A leg amputation and a lower jaw removal followed.Results arefirst presented to the medical community at the meeting of the Boston Society for Medical Improvements on November 9, 1846. Two days later, patent No. 4848 granted to Morton and his mentor, Charles Jackson, 10% of all profits from the surgical use of ether. This ismet with swift opposition from the medical community and isnot enforced.
- In 1853, the discovery of the hypodermic needle, the syringe, and the injection of morphine are innovations made possible by Alexander Wood. He invents a hollow needle that fits on the end of a piston-style syringe and uses the device to successfully treat pain by morphine injection. Note: Today, the majority of anesthetic drugs are delivered intravenously—which would not be possible without the invention of the syringe.
- Local anesthesia, in which pain is only blocked in specific locations, comes onto the scene in 1884 with the discovery of injectable cocaine. The renowned Baltimore surgeon William Halsted first injected 4% cocaine into a patient’s forearm and observed that the arm became numb only below the injection site.
- The first spinal anesthesia is also performed that year in Germany when Leonard Corning injects cocaine between the vertebrae of a 45-year-old man and causes the patient’s legs and lower abdomen to become numb. Note: Synthetic drugs will replace cocaine in the next century, with the discovery of Procaine (Novocain) and Lidocaine in 1905 and 1948, respectively.
- In 1891, the German physician Heinrich Quincke introduces the technique of lumbar puncture—later used to administer medications directly into the cerebrospinal fluid (CSF) during spinal anesthesia.
- The blood pressure cuff is introduced by Scipione Riva-Rocci in 1896.
20th Century
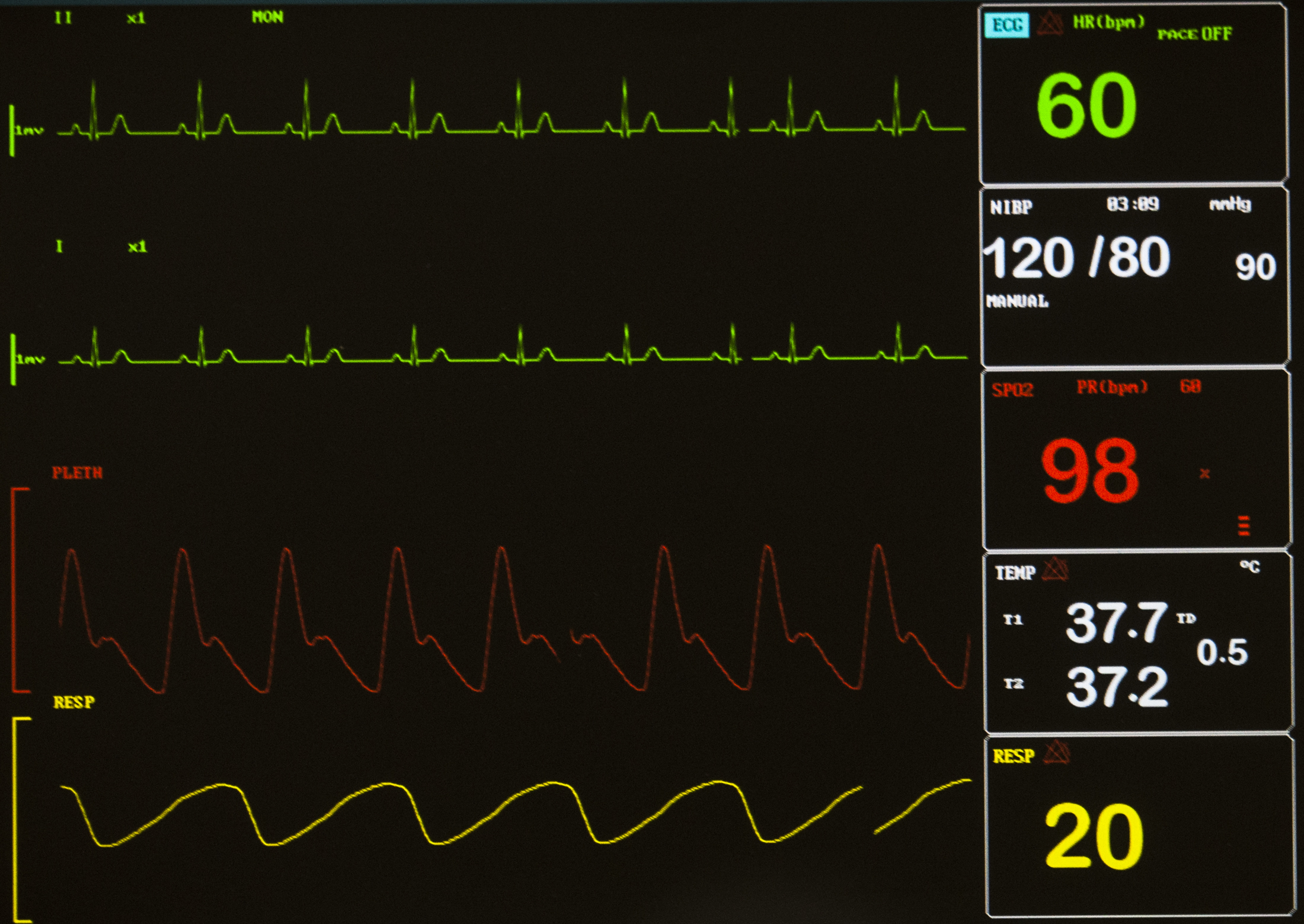
Once a patient is anesthetized, there is a critical need to closely monitor the body’s vital signs—pulse, respiratory rate, blood pressure, temperature, and oxygen saturation. This century heralded improvements in patient monitoring techniques, and a wider selection of synthetic anesthesia agents.
- The electrocardiogram is developed in Holland by Willem Einthoven in 1903.
- In 1905, a Russian physician describes the sounds—now bearing his name, “Korotkoff sounds”—heard through a stethoscope placed over a peripheral artery as a blood pressure cuff is deflated. This allows the systolic and diastolic components of blood pressure (BP) to be determined. This measurement gives the anesthesiologist important information during a procedure; a low BP may indicate anesthetic overdose, hemorrhage, or heart dysfunction, while a high BP may be evidence of patient distress due to inadequate anesthesia levels or uncontrolled hypertension.
- In 1913, endotracheal anesthesiais invented when Sir Ivan Magill develops a technique to place a breathing tube into the windpipe, and that same year Chevalier Jackson reports the ease with which using a laryngoscope allowed the insertion of an endotracheal tube. This was a landmark both for the field of critical care medicine because of its impact on resuscitation, and surgery, as operations of the abdomen and chest would not be possible without the ability to protect and control the airway.
- The cuffed endotracheal tube, which allows positive-pressure ventilation (PPV) into a patient’s lungs, is discovered in 1928 by two University of Wisconsin physicians, Arthur Guedel and Ralph Waters.
- Dr John Lundy changes the standard of care for inducing general anesthesia when in 1934 he introduces the intravenous anesthetic, sodium thiopental. Compared to the pungency of inhaled ether, a Pentothal injection was more tolerable and became the chosen method for sedation. Propofol, introduced in 1981, has since replaced Pentothal, but the delivery of anesthesia still almost always begins with the intravenous injection of some anesthetic drug.
- The American Society of Anesthesiologists is founded on Feb 13th, 1936.
- The paralyzing effect of curare became important as muscle relaxation was a necessary step to allow the insertion of endotracheal tubes. This ancient arrow poison was first deliberately applied to surgery by the Canadian doctor Harold Griffith in 1940.
- World War II and the Korean War battlefield medical inventions include shock and resuscitation units used to save the critically ill and wounded. Post-Anesthesia Care Units (PACU’s) and Intensive Care Units (ICU’s) are developed as extensions of these.
- Inhalation anesthesia is forever changed, when in 1956, British chemist Charles Suckling synthesizes halothane. Unlike ether, halothane has a pleasant odor, high potency, fast onset, low toxicity, and is non-flammable. Halothane replaces older “vapors” and is the forerunner to the modern inhaled anesthetics that followed: isoflurane, desflurane, and sevoflurane.
- Stanford anesthesiologist Dr. William New develops the Nellcor, the first commercially available device to allow pulse oximetry monitoring Prior to this date, it was not possible to measure a patient’s oxygen saturation and the first sign of low oxygen levels was often a cardiac arrest. A unique feature is an alarm that lowers the pitch of the pulse tone as saturation drops, giving providers a warning that their patients are in danger of oxygen deprivation.
21st Century
Today,modern anesthesiologists utilize dozens of medications and apply sophisticated high-tech medical equipment, requiring on average four years of training beyond medical school.What will the next “advance” be?New drugs, new delivery routes, and new delivery systems are the areas where research is focused. This includes:
- Transmucosal drug delivery—which can be nasal, buccal, ocular, rectal, and mucosal, and is similar to how a patch works, with the advantage that mucosal membranes are thinner and more highly vascularized so the onset of action is faster and the dose needed is lower.
- Intravenous anesthesia evolving towards a continuous drug infusion rather than an intermittent bolus approach. Related to this development is the optimization of Patient-Controlled Analgesia (PCA), a precision drug delivery technology enabled by an electronically controlled infusion pump which allows patients to self-administer (up to a prescribed threshold) until sufficient pain relief has been achieved. PCA has been found to result in less over-or under-dosing and more optimal drug delivery; patients also resume mobility more quickly and can be discharged sooner.
Interested in reading more on the topic? These are the sources referenced:
Anesthesia Fact Sheet. National Institute of General Medical Sciences Web site.http://www.nigms.nih.gov/education/pages/factsheet_anesthesia.aspxUpdated May 2015 Accessed October 7, 2015.
Eger II EI, Saidman LJ, Westhorpe RN .The Wondrous Story of Anesthesia.New York, NY: Springer; 2014
Timeline of important dates and events in the development of anaesthesia History of Anaesthesia SocietyWeb site.http://www.histansoc.org.uk/timeline.htmlAccessed October 7, 2015

