Klaus Schwab of the World Economic Forum calls it the Fourth Industrial Revolution; artificial intelligence (AI) and machine learning (ML) are poised to penetrate every industry, discipline, and economy, and health care is no different. A survey of healthcare executives by AI market research firm TechEmergence revealed that 50% of respondents believe that ML will be ubiquitous in healthcare by 2025.[i] As soon as next year, ML technology will be incorporated in 30% of health systems as tools assisting physicians in making personalized treatment decisions.[ii]
Though ML represents a disruptive force in the economy, particularly in the organization of human resources, understanding the technology and its limitations is crucial for healthcare stakeholders to direct its advancement for the benefit of patient care.
What is Artificial Intelligence and Machine Learning?
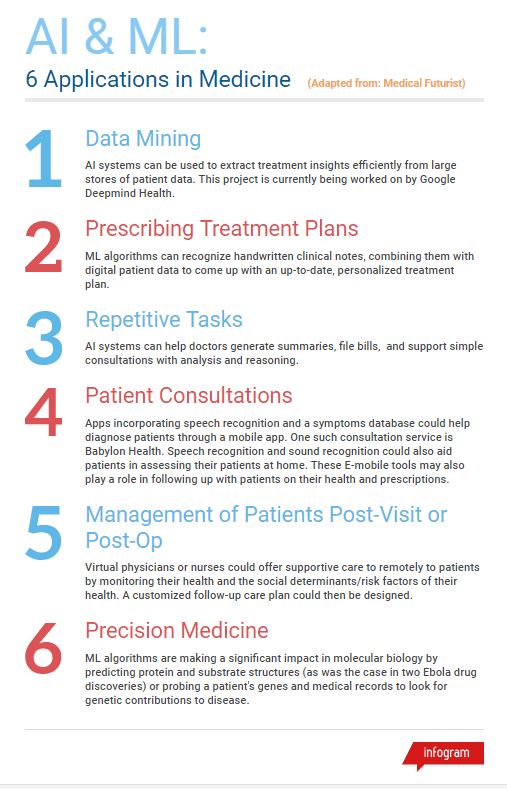
The field of AI is concerned with creating computer systems that are able to perform tasks normally requiring human intelligence, including but not limited to: visual perception; speech recognition; decision-making; and translation between languages. ML describes one approach to AI that uses algorithms beyond condition- or rule-based structure and “learns” from data to improve its performance. ML is concerned with creating algorithms that give computers the ability to learn from data and make predictions or decisions without being explicitly programmed. Major software and hardware advances that have enabled ML include parallel computing, the computing of simultaneous processes using multiple CPU cores, and the cloud, which allows for unprecedented access to large amounts of patient data (necessary for the training of some ML algorithms) and provides the computational capacity necessary for the development of ML models. One example of ML models include neural networks that are meant to conceptually imitate the structural cognitive pathways of the human brain).
ML in Healthcare:
The adoption of ML in healthcare is driven largely by big data (i.e. electronic health records, EHR) and personalized devices, effectively engaging ML development in a positive feedback loop. As medical futurist Bertalan Mesko, PhD, states, medical data is expected to reach 44 zettabytes by 2020, and the sheer task of managing that data will be best achieved by the implementation of ML tools.[iii] ML relies on big data, which will necessitate advances in ML to extract cogent conclusions from big data.
There are applications of AI in anesthesiology as well, and it isn’t unreasonable to imagine a system, through the cognitive processing of patient data, probabilistically and/or algorithmically making efficient and accurate decisions in “monitoring the depth of anesthesia, determining the amount of anesthetic gas to administer, somatosensory evoked potential monitoring, classifying patients, and mitral valve analysis to coding and billing”.[iv] By enabling data-driven physician and consumer decision-making, ML may play a key role in lowering healthcare costs.
However, there are important questions to consider with ML, as there are with any major technological advance.
Issue #1: Ethics in Practice
If a machine makes a mistake, who bears the ultimate responsibility? From an ethical and legal standpoint, it is substantially more difficult to hold an algorithm accountable for a “wrong decision”. This is because ML models are not explicitly programmed to make decisions based on certain conditions but instead have been developed to learn from data in order to devise treatment pathways optimizing patient outcomes. For a health care professional non-conversant in ML or computer science, the workings of such algorithms can feel opaque and inscrutable. In a clinical setting, a lack of understanding of the “thought process” behind an ML model may engender mistrust between technology and the people they were designed to help. Doug Marcey, vice president of technology for Plexus Technology Group, along with other healthcare consultants, indicates that the best way to approach ML use in patient care while avoiding these concerns is to keep the physician in the driver’s seat: “If you ask a doctor why they prescribed a drug, they can explain their thought process. A lot of ML models are just statistical. You can’t ask the model why it made a diagnosis or recommendation. That’s why, at least in the short term, we’re not going to replace people. We need someone at the helm who’s going to take responsibility.”
Issue #2: Infrastructural Readiness
ML algorithms are only as good as the data they are acting on, and electronic medical records still face barriers such as a high degree of heterogeneity of quality and network systems. Rural healthcare systems, which are traditionally slow to adopt EHR will also find it difficult to leverage ML tools.
Given that the penetration of ML in healthcare is all but inevitable, health care professionals should prepare by asking their practice, hospital, or management organization for the tools and expertise necessary to improving the quality of their data reporting.
Issue #3: Industry Resistance to Implementation:
In 2016, GE pulled Sedasys, its automated anesthesiology machine from the market, citing a lack of demand by hospitals and physicians. Resistance by health practitioners stemmed from a belief that Sedasys was the first of many disruptive innovations that will phase out human providers in favor of automated systems. However, such attitudes may ultimately prove counterproductive and ill-founded, at least in the short-term. “I think machine learning will become integrated into anesthesia, but will never replace the physician,” says Jody Locke, ABC vice president for anesthesia and pain practice management. “The big issue in anesthesia—and the big potential for machine learning in anesthesia—is risk stratification and identifying the potential for never events.” The vast majority of ML platforms, including IBM’s Watson Health are intended to serve as auxiliary tools to help physicians make decisions regarding patient care, or to perform tasks under the supervision of physicians. In order for this relationship to be productive and successful, physicians must embrace this technological shift and bring their perspective to bear on the utility of these ML platforms.
[i]https://www.techemergence.com/machine-learning-in-healthcare-executive-consensus/?utm_source=ABCeAlert&utm_campaign=ArtificialIntelligence&utm_content=6-12-17
[ii] https://www.forbes.com/forbes/welcome/?toURL=https://www.forbes.com/sites/jenniferhicks/2017/05/16/see-how-artificial-intelligence-can-improve-medical-diagnosis-and-healthcare/&refURL=&referrer=&utm_source=ABCeAlert&utm_campaign=ArtificialIntelligence&utm_content=6-12-17#273dcd716223
[iii]http://medicalfuturist.com/artificial-intelligence-will-redesign-healthcare/?utm_source=ABCeAlert&utm_campaign=ArtificialIntelligence&utm_content=6-12-17
[iv]http://www.anesthesiallc.com/publications/anesthesia-industry-ealerts/1037-ai-and-machine-learning-in-healthcare-and-anesthesia