
With the Affordable Care Act’s increased emphasis on improving the quality of patient care, the American Society of Anesthesiologists has offered the ‘perioperative surgical home’(PSH) as a new model for perioperative care delivery in which the anesthesiologist serves as the coordinator of care from the preoperative through the postoperative phase. The idea behind this organization is not only to increase patient-centeredness, but also to find opportunities to cut healthcare costs and improve the delivery of healthcare resources.
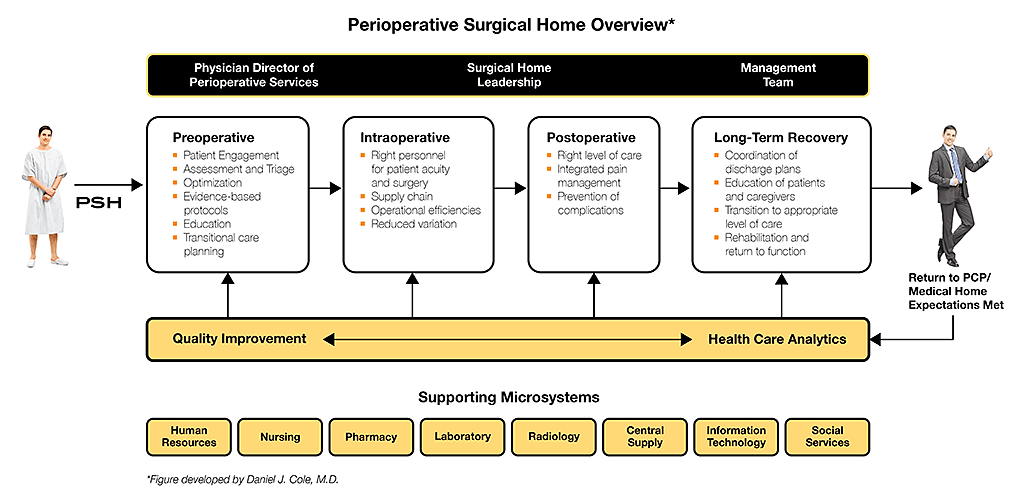
The PSH model aims to reduce variability in perioperative care given that variability increases the likelihood for errors and complications. One way in which this variability can be reduced is through assuring the continuity of care and treating the entire perioperative episode of care as one continuum rather than discrete preoperative, intraoperative, postoperative, and post-discharge steps. The PSH achieves this continuity by having one team headed by anesthesiologists, to manage all aspects of this continuum from the time that the patient and the surgeon make the decision for surgery until 30 days after discharge (See the figure below for more details). During this perioperative episode, the goal of the PSH is to ensure that best evidence/best practices are applied in a consistent and standardized way to every patient undergoing surgery. At each step of this continuum patients are informed, educated, and involved in the decision-making and treatment planning. The point is to allow anesthesiologists to have a unique opportunity to improve outcomes, decrease length of stay and other metrics, and improve patient satisfaction.
Since the concept of PSH was conceived, different versions of the model have been implemented at institutions across the United States such as the University of Alabama Birmingham Health System. Elsewhere, the UC Irvine Health System implemented a PSH for primary joint replacement surgery (hip and knee) with the support of the Chairs of Orthopedics and Anesthesiology and Perioperative Care and the Chief Operating Officer of the hospital. There, multidisciplinary teams consisting of anesthesiologists, surgeons, nurses, pharmacists, physical therapists, case managers, social workers, and information technology experts meet weekly during the implementation phase, resulting in decreased readmission rates during the 30 days following surgery (down to 0.9% from 3.0%).
The early results of PSH initiatives have been encouraging (e.g. decreased readmission rates, lower healthcare costs, fewer mistakes, more efficient allocation of healthcare resources). The model has significant implications for policymakers, payers, administrators, clinicians, and patients, and may lead to policy-relevant cost savings and quality improvement across the perioperative continuum of care – especially with respect to integrated care organizations, bundled payment, and value-based purchasing.

